My Third-Year as a Nursing Student



Throughout my nursing education, I have taken on the role of an unregulated care provider at Applefest Lodge Retirement Home as a UCP and a Clinical Extern at Northumberland Hills Hospital. These positions have granted me the opportunity to work within a changing environment as part of an interprofessional team where I have advocated for and promoted wellness while ensuring the delivery of safe, quality care.
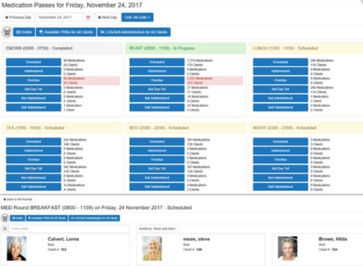
Skills I have learned while being a part of these organizations include: dispensing medications using an E-MAR, administering insulin according to a sliding scale, assisting with activities of daily living, communicating appropriately with patients and their families, transferring patients safely with mechanical lifts, and much more. I have also had additional time to become familiar with EPIC and practice charting concise and accurate information within a patient’s chart.

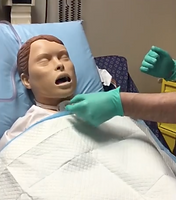
Throughout the 5 labs completed in NURS 3020, we practiced a variety of skills. Some of the skills taught were; IV piggybacking, head-to-toe assessment, manual BP, applying sterile gloves, in-dwelling catheter insertion (male and female), NG tube insertion, using a drug monograph, preparing injections (vial and ampule), wound packing and dressing, and drug reconstitution. The one competency that was pivotal to my nursing education, was having the ability to insert a male in-dwelling catheter on an actual patient. Although I was very nervous, overall I felt I was successful at my first attempt and will continue to practice and improve this skill.




Due to COVID-19 restrictions, there were a few occurrences we were not able to attend clinical. However, this did not halt our learning as we were given the opportunity to complete online simulations through CAN-Sim such as working with a complex COVID-19 case, fluid and electrolyte imbalances, and MODS. Although I enjoy learning in an environment where I am able to be hands-on, I feel more appreciate these additional learning simulations as it allows me to play more of a role in a complex situation with the safety of not having a real-life patient in my hands. These modules have demonstrated the importance of personal safety while caring for a patient with COVID-19 and which interventions are most appropriate for these cases.

During my second year of the compressed nursing program, I took advantage of the opportunity of being on the TFNSA board for the year 2021-2022. My role in this organization is the Compressed Stream Representative where Ihelp organize and host events and will be apart of the 2022 pinning ceremony.
The Beginning of NURS 3020
Thursday, January 13, 2022 (B6, 8 hours)
Today marked the first day of clinical in the acute care rotation. It was an early morning start as I woke up at 0420 hours to be at PRHC for 0630. When I arrived, I met my preceptor, Jovette, and group members whom I would be working alongside on B6, a med/surg floor. Our shift started in the cafeteria where we went over general expectations and how the day would run. We then made our way to the unit where we were assigned to a nurse. I had the pleasure of shadowing Annika, herself is a recent RN grad from Nippising in 2020. We were assigned to 4 patients, 2 experiencing delirium, 1 with C. diff, and 1 who had CHF. All my patients were ladies and very pleasant to care for. The first nursing skill I put to use was taking a set of vital signs where I regrettably admit I had an uncomfortable time counting respirations. This is something I want to become more confident in. I then bathed the lady with C. diff which was comforting for me as this is something I am used to from working at NHH. We then set our patients up for breakfast and took a little tour of the floor. I also assisted in another nurse’s patient assignment where I helped gentlemen use the bedpan. This was also an uncomfortable situation at first as he had told me he had been admitted for attempting suicide so I had to be mindful and therapeutic in how I responded to his situation. Before heading for our own breakfast, a group member had the opportunity to observe a barium swallow procedure on a very sad case. This is where a patient is fed different thicknesses of food and contains a barium dye so that their swallowing can be observed through an x-ray. Unfortunately, our patient was not successful at eating some foods safely and did not have the proper reflexes to rid his airway of the substances. After watching this procedure, we then had some time for breakfast where we got to know our group members a bit better. The girls I am placed with seem very nice and a group of people I will get along well with! We then headed back up to the unit where I was able to quickly wash another patient’s hair as she was going to be going home later today but was pulled away as we were scheduled for a “debrief” meeting. Here we found out more information about Jovette and her diverse nursing background. We also gave an overview of ourselves and discussed some further expectations. We then headed up to the unit one last time where I sat and talked to a dementia patient who enjoyed sharing his passion for cars and then finished the day doing a scavenger hunt around the unit. This was a good activity to demonstrate how well we worked together as a team. It will be interesting to see what tomorrow has in store.
Friday, January 14, 2022 (B6, 8 hours)
Going into day 2 of clinical, I was indifferent. I felt the majority of tasks I had been doing were similar to those that I am responsible for in my externship. When I arrived at the hospital, we were quick to go into the unit and start shadowing our new nurses. Today I was with Jenna who is an RPN and is currently taking her RN at Nippising as well. She was very patient, resourceful, and did not cut any corners when caring for her patients. My patient load was similar to yesterday. I had 2 dementia/failure to cope patients and 2 AKI. The patients with AKI were unique as one had also attempted suicide, which was another primary reason for visiting the hospital, and the second was a chronic alcoholic who is frequently readmitted due to her progressing liver failure. When caring for one of the dementia patients, I learned how to safely and appropriately use lap and wrist restraints. He was not aggressive, however, he needed to be restrained while performing peri care and eating. I was also able to use some of the techniques I had learned in SafeMedicate where I needed to calculate the appropriate volume for a SUBQ injection. One improvement I would like to highlight was my ability to count respirations without the patient knowing and create my own flow of how I take vital signs and meet the patient for the first time on shift. The major skill we focused on today was a head-to-toe assessment. I was very nervous to complete this as I had only practiced on the computer with Shadow Health. The patient I chose to do my assessment on was the AKI patient who struggled with alcoholism. My clinical instructor was very patient and knowledgeable when watching me perform this skill. I was able to better listen to cardiac sounds and landmarks better, hear abnormal breath sounds due to the distention in her abdomen, and palpate an inflamed liver. These examples made me more aware of the human anatomy as I was able to see it in “real-life” and also taught me some of the complications and abnormalities to be aware of in the future. During the assessment, the doctor came in to talk to our patient. This was a very uncomfortable moment as palliative care vs. active care treatments were being discussed, as well as a potential new issue of a bowel obstruction. Here I was able to build a therapeutic relationship with my patient and Jovette helped me provide resources for our patient to use (such as social workers, psychologists, and reaching out to the nurses for extra support). Today truly demonstrated how a thorough head-to-toe assessment can be vital for monitoring the progression of symptoms, how much information can be learned just through communication, and how compassion and empathy are important qualities to have when building a trusting relationship with your patients.
NURS 3021
Midterm Evaluation




Drug Cards
Skills Lab
 |  |
|---|---|
 |  |
 |  |
 |  |
 |  |
 |  |
Elsevier Skills
-
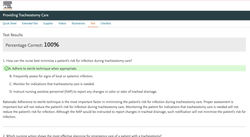
Providing Tracheostomy Care
-
Performing Nasotracheal and Nasopharyngeal Suctioning
-
Performing Oropharyngeal Suctioning
-
Collecting a Sputum Specimen
-
Performing Oral Hygiene for an Unconscious Patient
-
subcutaneous link insertion
-
pronouncement (post-mortem body care)
-
Inserting a Nasogastric Tube
-
Managing a Nasogastric Tube
-
Performing Gastric Occult Blood Testing
-
Providing Enteral Feedings
-
Removing a Feeding Tube
-
Taking Aspiration Precautions
-
Assessing the Ears
-
Assessing the Eyes
-
Assessing the Head and Neck and Lymphatics
-
Assessing the Neurologic System: Motor and Sensory Functions
-
Performing Blood Glucose Testing
-
Administering Subcutaneous Injections
-
Drawing up More than One Type of Insulin
-
Preparing and Administering Insulin
SIM 1&2
Elsevier Skills
-
Performing sterile gloving
-
Adding items to a sterile field
-
Pouring a sterile solution
-
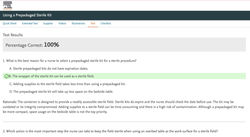
Using a pre-packaged sterile kit
-
Changing a dressing
-
Documenting medication administration
-
Preventing medication errors
-
Ensuring the six rights of medication
-
Using an automated dispensing system
-
Administering subcutaneous injections
-
Administering intradermal injections
-
Administering intramuscular injections
-
Administering oral injections
-
Assess pain
SIM 1&2 Preparation
SIM 1&2 Drug Cards
SIM 1 Pre-Survey
SIM 1&2 Post-Survey
 |
|---|
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
SIM 2 Pre-Survey
SIM 3 Post-Survey